Therapize Me?
“I think you should consider seeking therapy,” I said to a friend, midway through a conversation that would end disastrously.
We were sitting on the couch in our common room, like we did most nights. It was late; I was tired. The pauses between beats in our conversation lengthened into heavy silences, disturbed by the occasional hallway door slammed shut.
She was struggling with anxiety related to a problem that would likely persist for the next month, one beyond either of our abilities to fix. I cycled through the usual, trite suggestions: getting more sleep, taking it easy with work, talking with her family. All were summarily dismissed. Finally, I suggested therapy because I couldn’t think of any other way to help her.
Immediately she grew reticent and eventually visibly angry. She accused me of implying that she was incapable of managing her own problems. I was aggressive and uncompromising in disabusing her of this notion, which I saw as internalized stigma toward mental health. “Other people can get therapy,” she insisted, “but it’s not for me.” We didn’t get anywhere.
Eventually she got to the root of what upset her: She believed that I had suggested therapy because I felt burdened by her emotions. “I’ll stop talking about this,” she offered — the opposite of what I wanted. But that conversation would be one of the last times she opened up to me about her mental health. It marked the inflection point in a gradual distancing.
My impulse to suggest therapy has haunted me ever since. I recommended therapy to her without any idea of what it would entail: how long it might take her to get it, what treatment she could receive from Harvard, if it would be effective. I only knew that she shouldn’t be ashamed to talk about it.
We had lived together for months before the pandemic, Zoomed everyday during it, and lived together after. Now, she has stopped speaking to me entirely.
It makes me wonder: What kind of care do we owe our peers? How do the lines between peer and caregiver blur? And on Harvard’s campus, what does it look like to get help?
***
At this point, we know beyond a doubt: The kids are not alright.
Over the past few decades, mental health problems, especially among young people, have reached epidemic levels. As Howard E. Gardner ’65 and Wendy Fischman, two researchers at the Harvard Graduate School of Education, write in their new book “The Real World of College,” mental health is the defining issue on college campuses, and it has been for the last ten years.
Rates of depression, anxiety, and serious suicidal ideation among college students have doubled over the last decade. A 2020 report authored by Harvard’s Task Force on Managing Student Mental Health found that from 2014 to 2018, the percentage of undergraduates who said they struggled with depression jumped from 22 percent to 31 percent, and for anxiety, from 19 percent to 30 percent. Only 34 percent of students reported feeling comfortable seeking professional help for emotional problems. (The report names several issues likely contributing to poor mental health, including overwork, loneliness, competitive extracurricular activities, imposter syndrome, and stigma against seeking help.)
Nationwide, the Covid-19 pandemic only increased this burden — which hasn’t lessened even though pandemic restrictions have eased. The Harvard Kennedy School’s Institute of Politics’s recent Youth Poll reports that more than half of young people continue to experience feelings of depression and hopelessness, with no statistical differences based on age, race, or ethnicity.
At Harvard, Counseling and Mental Health Services is the Harvard University Health Services division devoted to providing mental health support and resources. But some students have taken to social media and publications to decry CAMHS’s failures to meet student needs.
A recent post on Harvard Confessions, an anonymous student Facebook forum, details the agonizing process of trying to find a therapist through CAMHS: “It has been the most frustrating, confusing process to get one. I have tried all their services meanwhile but every single interaction has been awful… I’m tired of this process, I just want help.” While I can’t corroborate the experience of the source, the post is representative of broader anti-CAMHS social media discourse. At a 2018 town hall, following an incident in which the Cambridge Police Department arrested a Black Harvard student in need of mental health care, students upset with long wait times demanded CAMHS hire more therapists; in March of this year, The Crimson reported that the wait time for new patients to book an appointment was about 6 weeks.

Students have also alleged that CAMHS is not racially diverse enough in its staffing and resources. In 2015, just one quarter of CAMHS counselors were people of color, prompting Black students organizing for social change to demand the “expedited hiring of more Black and Brown counselors.” Last year, following a rise in anti-Asian violence nationwide, CAMHS faced backlash over its “Anti-Asian Racism Resources” page, which told Asian American students that “you may wish that you weren’t Asian, but remember that your ancestors likely went through similar or even worse incidents.”
Despite these criticisms, students are, at least in my experience, still quick to recommend seeking CAMHS or trying therapy in general. Over meals and brain breaks, in common rooms and libraries, I’ve heard CAMHS offered as a next step. Discussion around therapy on campus rarely extends past this, rendering CAMHS either a scapegoat or a catch-all solution for anyone struggling. This obscures the actual process of obtaining therapy, as well as the full range of mental health infrastructure on campus — let alone what the future of mental health care could or should look like.
Before writing this piece, I had never been to therapy myself, nor had I ever felt like I needed it — but I had recommended it to other people, like my friend. While I have my share of social and academic challenges, I am fortunate in that I haven’t been affected severely by mental health issues. As a consequence, it occurred to me that I would only think to seek mental health resources for myself when I imminently needed them, at which point the resources might be too little, too late.
In an effort to lift the veil on mental health infrastructure on campus, I went through all the steps of seeking support — CAMHS, private therapy, peer therapy organizations, and broader spirituality and wellness oriented spaces — to comprehensively evaluate the full network of care available. (I went through the motions of obtaining resources that were zero-sum, like CAMHS and private therapy, but did not actually use them, lest I be taking them away from someone who needed them.)
The irony in this project is that I could only go through all these steps of seeking care because I was mentally well enough to try and had the time to dedicate to it, which is likely not the case for many students. I also can’t represent students struggling with severe mental illness through my own experiences, nor is that my intention. I am just one person, but I believe my efforts can help illuminate what it takes to get mental health care and what that care actually looks like in practice.
In addition to taking a critical eye to current resources, I also sought students and faculty who have visions of what the future of therapy, and mental health care more broadly, might look like on campus. What would accessible, meaningful, comprehensive mental health care at Harvard entail? How can our existing services be used in concert to provide a more tailored safety net for students? And what responsibility does the University have in providing this network of care?
***
To evaluate existing resources, I started with what many students see as the first line of defense: CAMHS.
CAMHS provides one-on-one counseling, as well as workshops, listicle-style advice, and referrals to local therapists. As per its mission statement, CAMHS aims to “respond quickly and in proportion to the student’s or administrator's expressed need” and “collaborate with the student to create and implement a plan that allows for increased perspective, growth and a return to a level of functioning most likely to promote success at Harvard."
As of March, CAMHS employed 36 clinicians trained to offer a variety of treatments, from trauma-informed therapy to Cognitive Behavioral Therapy, a form of talk therapy meant to help the patient identify and respond to inaccurate or negative patterns of thinking. CBT is used for anxiety, depression, and insomnia, some of the most common conditions that affect students.
This past fall, over 3,000 students had clinical appointments with CAMHS. In July of 2021, CAMHS also launched CAMHS Cares, a 24/7 support line for students who needed urgent care. During the pandemic, as demand for therapy rose, the support line was receiving hundreds of calls a month.

To make a CAMHS appointment, Harvard students must go through the HUHS portal and book a phone consultation.
It takes me an embarrassingly long period of clicking to get to this booking portal — I only use HUHS about once a year to upload my immunization forms.
After specifying that I’m not a varsity athlete, I reach the mental health question:
“In a few words, let us know your concern [30 char limit]”
I start typing “In the last few weeks” and realize the severity of the limit. It seems impossible to fit anything detailed or cogent in the response box. I decide to leave it at “anxiety and stress.”
But when I try to book a consultation, the earliest one available is on May 3, and the earliest I can feasibly make is on May 5: three weeks away. And that’s just the consultation — presumably there would be another intervening period between the consultation and actually receiving therapy. Most of the things on my mind — the housing lottery, final assignments, summer deadlines — would have to be resolved well before then. I would be lucky if I got therapy before the end of the semester.
I close out the tab.
***
For me, this long wait time was a nuisance; for others, it can be a serious barrier to accessing needed care.
After struggling with “lots of anxiety” throughout freshman year, Lauren V. Marshall ’22 tried to get a CAMHS appointment at the beginning of her sophomore year. She made an appointment through the CAMHS portal online, but their earliest availability was a month or two away — and again, that was just for the consultation.
“I thought it would be the first appointment,” she says. “They didn’t make that clear.”
After her consultation, CAMHS connected her with a therapist, but then Covid-19 happened, and that resource evaporated. A year later, when she came back to campus, Marshall finally contacted the therapist.
Even then, she decided to stop after only a few appointments. Her therapist, likely using some form of CBT, expected a lot from her, she says. It was a style of therapy she didn’t believe was benefiting her. “I’m not good at asking for help, and the therapist put that burden on me,” she says. She feels an irony in this: “My stress was having too much to do. If the solution is doing more stuff, that’s not ideal,” she says. She sought therapy for her stress, but the time-consuming, bureaucratic process of getting it only added to that stress, and the form of the therapy wasn’t compatible with her needs.
According to Barbara Lewis, the chief of CAMHS, the average number of CAMHS appointments a patient receives is about four, suggesting that even for students who do score an appointment, CAMHS therapy is not a long-term solution.
Lewis is explicit about this, describing CAMHS as “short-term solutions focused,” although students are not automatically assigned the same number of appointments. According to the CAMHS website, “Some students feel benefits after one to six sessions, others need more time.”
But Lewis says she’s “not content” with wait times and overall student satisfaction, and that CAMHS is working on implementing the recommendations of the 2020 Mental Health Task Force. She also emphasizes the success and low wait times of the CAMHS Cares line.
“Just talking to someone in that moment staves off a crisis,” she says. (Personally, I didn’t try the hotline, as part of my commitment to not using zero-sum resources.)
CAMHS does offer same-day urgent appointments for students in crisis, as well. “If students need to be seen in-person, we will get them in,” Lewis says.
But for non-urgent cases — anyone in mild to moderate distress, like me — you can’t count on getting a CAMHS appointment quickly, trying to get one is itself taxing, and there’s no guarantee that the care will be quite what you need.
***
It’s a familiar refrain: If Harvard has so much money, why don’t we just hire more therapists?
To get an answer to this, I spoke with Steven E. Hyman, a biology professor who served as the University provost from 2001 to 2011. He also led the National Institute of Mental Health from 1996 to 2001.
During his tenure as provost, he observed that campus mental health issues were “overwhelming for us and all of our peer universities.” A 2004 investigation by The Crimson had found that almost half of Harvard undergraduates had experienced depression that inhibited their daily function, prompting students to criticize the inadequate supply of mental health resources.

But according to Hyman, beefing up the supply of therapists ran up against a budget constraint — the University could only afford to hire a limited number of mental health professionals without raising the Student Health Fee. Required for all registered students enrolled more than half-time in Massachusetts, the Student Health Fee covers HUHS services — like CAMHS, flu clinics, and alcohol and drug services — in lieu of insurance, says Lewis. It stands at $1,304 for the 2022-2023 academic year, a marginal increase from the last few years.
Under this funding structure, the cost of hiring more therapists could come directly out of students’ pockets. “There was a concern about the total cost to students who were healthy,” Hyman says. “It’s just really hard to free up money internally.”
Lewis suggests CAMHS is looking for other sources of funding, but she would not elaborate on what these might be.
Since Hyman’s years as provost, shortages have persisted, and reports show student mental health has deteriorated — trends the pandemic only exacerbated. On top of the hundreds of phone calls to CAMHS Cares and the recorded uptick in student depression and anxiety, Lewis describes “huge turnover” last August as CAMHS therapists left, some moving to private practice. They’re “almost up to full capacity again,” she says, but still down some staff. In March, The Crimson reported that CAMHS employed 36 clinicians, an increase from 32 during the pandemic, but still fewer than in 2018, when it employed 41.
Perhaps raising money specifically for mental health could be an end-around the funding crunch, Hyman suggests. “I think there would be donors. Every family has been touched by this,” he says. And Lewis points out that the CAMHS Cares line is funded entirely by a donation. Much University fundraising takes place behind closed doors, so it’s possible that more donations could continue to improve care.

But without a dramatic increase in funding, the existing bottleneck will continue to block much-needed services. “People would come to us asking us to support screening campaigns,” Hyman remembers, referring to preventative mental health diagnoses. “I would say, you know, it’s great, but what if somebody screens positive? Do you actually have a place for them to get help? Or are you screening people into the void?”
***
With CAMHS a long way off, I wanted to see if outside therapy was a feasible option. Google seemed like a good place to start. I searched “therapy near me.”
A bunch of ads popped up, followed by Yelp: “The Best 10 Counseling & Mental Health in Cambridge, MA.” I clicked through a few of them. Some were too far away. None were cheap. Mount Auburn Counseling Center, for example, costs between $75 and $175 for a single session. Through ThriveWorks, a site that pairs individuals with local therapists, I found more options, similarly expensive. BetterHelp, a similar site, found the average price range of a therapy session in Cambridge to be $85-$150 and listed “more affordable options” as $60-$90. Many therapists I found online weren’t taking new patients, or weren’t taking them for a while. Some of the cost could be covered by my insurance, but I didn’t know how much, and I couldn’t assume the same would be true for other students. Given that I was intimidated by the insurance process, and I didn’t want to spend hundreds of dollars a semester or travel a good distance to get care, private therapy seemed out of the realm of possibility.
The lack of available private therapists isn’t separate from the University’s therapist shortage. Hyman points out that even with sufficient University funding, there simply aren’t enough therapists to go around. Nationwide, the pandemic exacerbated a preexisting shortage of mental healthcare providers — as demand for therapy increased, burnout among healthcare providers did, too. Locally, Cambridge Health Alliance, a major healthcare provider serving Cambridge, Somerville, and Boston, lost dozens of therapists and social workers last fall, for example.
“In Cambridge, Massachusetts, the number of therapists outside of the University who are well trained in CBT and who take insurance are very few,” Hyman says, confirming the trouble I had finding a therapist online. Hyman explains that the shortage exists because of poor reimbursement, especially for therapists who take insurance. “People who skillfully do psychotherapy also have to eat and live,” he says.
In some cases, Cambridge residents face even longer wait times than Harvard students. “The thing that makes my heart sink is when a colleague asks me for a referral for their child, and people say, ‘Oh, yeah, I can see them in six months,’” Hyman says.
And if Harvard hired more local therapists, they would come directly from this already-limited pool of local therapists. “It is zero-sum,” Hyman confirms. “It depletes outside therapists, absolutely.”
He paints an ugly, grim picture, one no amount of funding could solve: There aren’t enough hireable therapists for CAMHS to address all student needs — CAMHS is constrained to function as a short-term stopgap for people in crisis. For students who would benefit from long-term support but are not in dire need — like Marshall, or like my friend — Harvard would be hiring counselors at the expense of other Cambridge residents. The one-on-one therapy system is neither expandable nor sustainable.
At this point, I felt I’d exhausted on- and off-campus professional counseling. It was time to turn to the alternatives.
***
In 1971, Margaret McKenna ’70, a recent Harvard graduate and teaching fellow, founded a new therapy organization to address gaps in mental health infrastructure on campus. Called Room 13 after its address in Mather House, McKenna described it as “something in between talking to a friend or roommate and seeing a psychiatrist.”
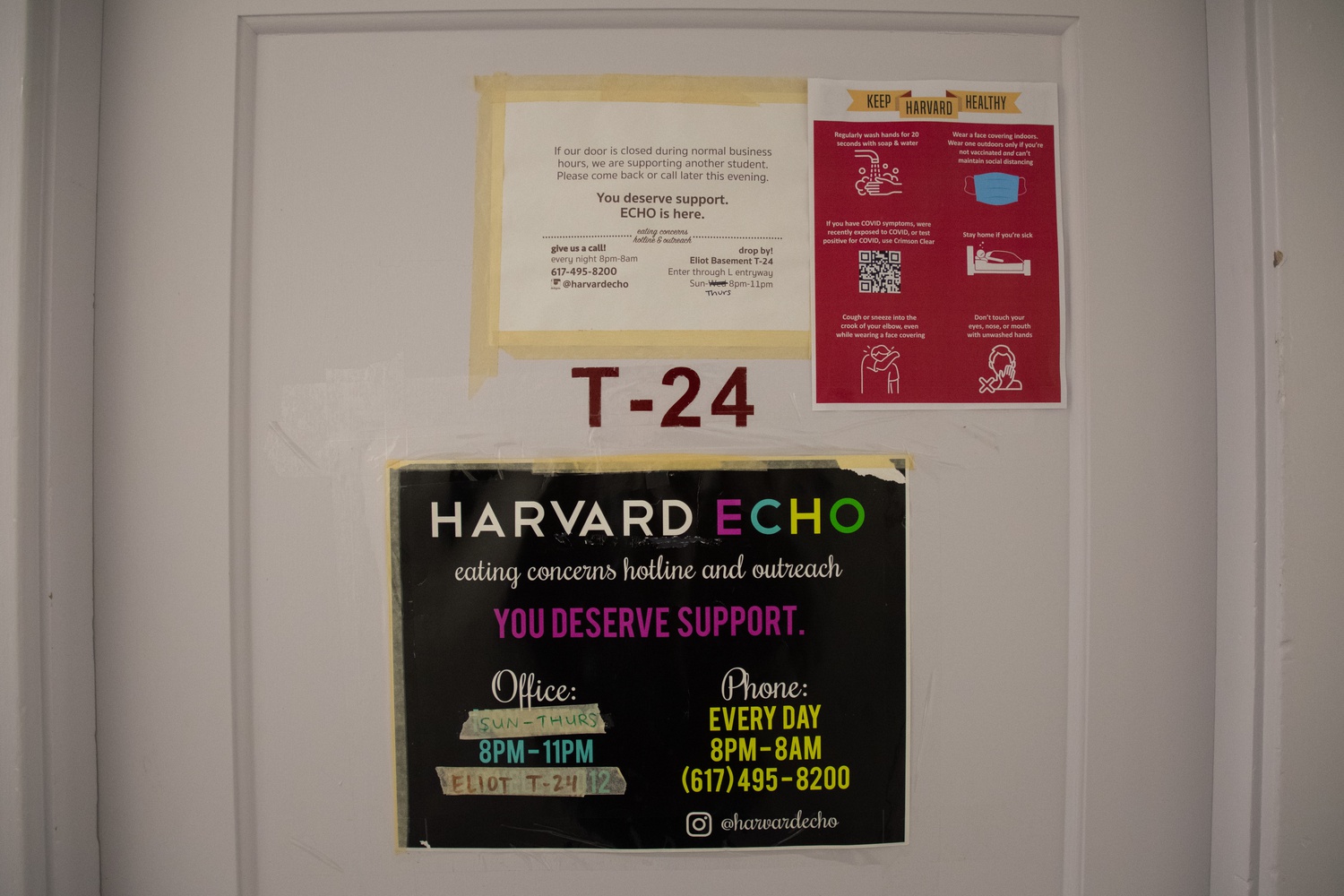
Half a century later, Room 13 is still in operation, and their flyers, which read “Feeling stressed, lonely, angry, anxious, overwhelmed?” are ubiquitous. Room 13 is now one of five peer therapy groups supervised by CAMHS, which serve as another line of defense for students who struggle to seek professional help.

Other, issue-specific peer therapy organizations have emerged: Contact, which focuses on BGLTQIA+ identities; Eating Concerns Hotline and Outreach, which focuses on eating disorders and body image; Indigo, which focuses on identity and intersectionality; and RESPONSE, which focuses on sexual assault, intimate violence, and relationships. Some of the groups, including Room 13 and Echo, offer hotlines in addition to their drop-in hours. According to a Contact counselor, all the counselors receive 25-30 hours of training from CAMHS and their organizational directors in the weeks before their first semesters; the training involves a mix of informational content, role playing, and safety requirements.
“I don't know how many people will call,” McKenna said to The Crimson when Room 13 was first formed. “This place is so lonely and people’s pride is pretty ingrained. But there are people around this university who care, and we're trying to demonstrate that.”
Peer therapy is accessible, staffed with trained counselors, and freely available. In other words, it seems to offer a solution to many of the issues I found in CAMHS and private therapy, especially for students with less severe but still time-sensitive problems. CAMHS recommends students try peer therapy to get the support they need. I decide to give it a go.
***
I begin with Room 13. On a Tuesday evening, I approach Thayer, a freshman dormitory, with the feeling that I am casing the premises for a break-in. My ID doesn’t work on the door I try, so I follow a freshman after he swipes in; he eyes me suspiciously.
Once I’m in Thayer’s basement, the room is easy enough to find. A sign encourages me to knock, so I do; I am greeted by two student counselors who gently but efficiently usher me into an adjoining room. It is the beginning of their hours, so I assume I am their first client of the day. Neither counselor asks for my name, and I don’t ask for theirs. No real adult is present, nor any kind of documentation, like a sign-in sheet. The system is clearly designed to ensure privacy and anonymity.
The adjoining room is painted a yellow-beige, dimly-lit, and warm, womblike. We all take off our shoes. Something about the room surprises me. I expected to see my high school guidance counselor’s office: claustrophobic, bowls full of fun-sized candy, walls replete with mindfulness posters. Instead, it’s spacious, and the walls are decorated with minimalist landscape paintings. There’s a bed behind the couch cushions; it’s unclear who sleeps on it. I have a vision of someone reclining all the way back, to the intonation of So how does that make you feel?
Both counselors sit across from me, cross-legged on two armchairs. They say I can talk about anything, so I let them know it’s my first time here, and while there’s nothing particularly big happening in my life right now, I want to be proactive about my mental health. But midway through a sentence, I start crying.
This is unexpected; I rarely cry. The counselors ask questions to determine what is weighing on me. Out comes a list: I didn’t do so well on a midterm last week, I have to deal with the housing lottery, which relates to a difficult situation with one of my roommates, I am balancing a lot of deadlines, et cetera.
They only ask open-ended questions, the vast majority of which are about how actions or realizations made me feel. We talk a lot about my feelings toward my ex-friend and my obsession with grades. As I talk, I feel calmer, lighter; I stop crying about ten minutes in, but there’s no real way to keep track of time, and I realize I have no idea how the session is supposed to end. One of the counselors leaves. The other counselor continues asking questions, and I continue answering them. She offers neither feedback nor advice — not even anodyne consolation, like “That sounds tough.” Just the questions. At first this is slightly irritating in its one-sidedness. But I soon find the rhythm has a certain appeal: The counselor does not have to share herself, and I do not have to feel like I am talking too long, or taking up too much space. Unlike my friends, she feels no need to offer solutions. The simplicity gleams: I talk, she listens.
***
After Room 13, I also try Contact and ECHO. All of the groups follow the same pattern: I walk in, they ask questions, and I answer them. I came to realize that rather than using CBT like many CAMHS therapists, they all employ a non-directive, open-ended form of therapy called Rogerian therapy, in which the patient reaches insights about their thinking and behavior through answering questions rather than receiving guidance.
Other commonalities I find: All of the groups are somewhat difficult to find, and decorated in a similar way, with landscape minimalism, lamps, and pillows. The vast majority of the counselors I interact with are women. I know many of them to varying degrees.
My sessions in peer therapy were mostly positive: I believed that the counselors cared, and were listening — like talking to a friend without the burdens of friendship. Even if it didn’t help me resolve the issues I was dealing with, or understand them better, peer therapy simply felt good to do, a kind of unburdening. Recognizing it might work more for others than it did for me, I would (and did) recommend it to a friend.
And yet, what struck me most was its underutilization, even though CAMHS is egregiously oversubscribed, and the therapy groups attend to overlapping issues. Again, numbers aren’t available for this, and many peer counseling groups have a policy against speaking with journalists, so I have to rely on my own experience: When I visited Room 13, only one other student came in during my hour-long stay; at ECHO and Contact, no other students sought care during my visit. It’s certainly not for a lack of advertising — the groups’ flyers are omnipresent, papering bathroom stalls, bulletin boards, and email lists.
I asked Marshall, a student who sought therapy from CAMHS, why she never tried the peer groups. “It didn’t really seem like an option,” she says. In conversations with friends, many of them — including some who had sought help from CAMHS — had never really considered using the peer groups. They were concerned about compromised anonymity, and uncertain about the rigor of training the groups received. The distrust seemed to reside somewhere in the dissonance between “peer” and “therapy.”
As for me, though I recognized the value of peer therapy, my visits also made me aware of its limitations. Knowing some of my counselors — especially knowing some of them were younger than me — diminished my willingness to be therapized by them: I had unfair reservations about their capacity as therapists because I knew them first as people. And even when I didn’t know the counselors, the dynamic still felt strange; this peer was now someone I could not be friends with, given the patient-therapist relationship that would always precede any friendship. I also didn’t like that all the counselors were women: Although I could not acquire demographic data on the counselors, and may have experienced a biased sample, it seems that female students are doing a disproportionate share of the emotional labor tied to this kind of work.
It seemed to me that the peer groups were conducting a version of traditional, therapist-patient care, except that the counselors were, of course, not professional therapists. And as much as I enjoyed my experiences with them, I could not bring myself to believe that the counselors could truly help me.
***
At this point, I had tried CAMHS, private therapy, and peer therapy. I felt that there were gaps in this network of care, and I hoped to find something that captured the peer support aspect of peer therapy, and that feeling of unburdening, without the constraints I had felt with the peer groups.
I spoke about this dilemma with Meredith Johns ’23, a friend of mine who sought therapy freshman year, following the death of her brother. She started with CAMHS but eventually moved toward alternative forms of care.
She was in Atlanta over break for her brother’s funeral, and she reached out to CAMHS to make an appointment ahead of coming back to campus. “I thought that was the responsible thing to do,” she recalls.
She tried to book a CAMHS appointment online, but none were available. So she called.
“They said: ‘If there are no appointments, there are no appointments.’ Or something very close to that.” She laughs a little. “And I said: ‘My brother died a few days ago, and I would really like to talk to someone.’ And they said okay.”
Johns had a few appointments at CAMHS, but eventually stopped seeing the clinician — “in a pretty non-dramatic way,” she qualifies. Though she says there was nothing wrong with her CAMHS experience, per se, she felt she needed something more specific to dealing with grief.
She started attending “a very woo-woo bereavement group” associated with the Harvard Divinity School. The group met about five times over the semester, in a room at the top of Memorial Church.
Some of her experiences seemed comparable to the peer therapy organizations on campus. “It was very talky,” she says. “Which at the time was good, and is maybe still how I process.”
But unlike peer therapy, the group had an ecumenical bent. For Johns, participating in the group was the start of her broader reorientation towards spiritually oriented care: She started going to Quaker meetings and taking religion classes.
“I got to keep asking why people suffer, while I was suffering the most I've ever suffered, in a way that I had trouble connecting with people about.” She pauses. “Yeah, therapy just didn't do it.”

Given Johns’s emphasis on religious and spiritual spaces, I decide to seek out counsel from a religious leader in a religious space, although I am not religious myself. On a Thursday afternoon between biology class and lunch, I go to confession at St. Paul’s Parish, the Catholic church in Harvard Square, and I speak to a priest, both about how I am doing and about how his work could be a form of mental health care.
He affirms the value of therapy, but he makes clear that he sees his work as distinct. “Therapy is about body-mind integration,” he says. “I also touch on the spirit.” His words echo Johns’s comments — this idea of a third dimension of selfhood that therapy can’t quite reach.
We shift to discussing my current quandaries, and I tell him about my difficult roommate situation. His counsel: “Sometimes what grates on other people is our defects. We must strive to eliminate our imperfections.”
This surprises me. So far, no one I received care from has told me to change anything about myself or given me clear, firm advice. Unlike the unflinching positivity of friends and the non-directive questioning of the peer groups, he was willing to suggest that I had problems — something that seems essential to making progress.
But in the confession box, we were still conforming to a particular model of mental health care: isolated, one-on-one, caregiver and care receiver. And for the plurality of students who don’t identify as Catholic (myself included), or even as religious, this form of care is limited in its helpfulness; the priest couched much of his advice in Catholic doctrine.
I get the sense that it’s not simply the religious aspect of Johns’s bereavement group that mattered to her — it’s the community attached to it, the feeling of embeddedness and mutual care.
“I actually think one of the main things I got out of that space was affirmation or validation from peers, and especially slightly older peers, that I was doing vaguely the right things about mental health and grief,” Johns says.
So what would such a community look like if it were secular?
***
Every week, a group of 6 to 8 students gathers around a table, with no one sitting at the head, to talk about their mental health. This is Harvard Undergraduate Group Peer Therapy, a newly-founded student organization. Each session, they start by filling out the GAD-7 (General Anxiety Disorder-7) and PHQ-9 (Patient Health Questionnaire-9), forms that measure anxiety and depression respectively, and they map their fluctuations throughout the semester. The atmosphere is quiet, relaxed. But over the course of the 75-minute session, as they discuss both their relationships and one of four topics — role transitions, interpersonal disputes, grief and loss, and isolation — they become more animated. When HUGPT first convened, at the beginning of fall semester, many of its members were relative strangers. Now, they discuss their weeks with intimacy and vulnerability.
Unlike the other peer therapy organizations, HUGPT works at the level of a group, with no counselor-patient central dynamic. HUGPT uses Interpersonal Psychotherapy, rather than Rogerian therapy or CBT. According to their website, IPT is based on two ideas: that mental health is largely determined by people’s relationships, and that relationship health is primarily driven by the communication of needs and emotions. “Nobody communicates their emotions perfectly,” the website reads, “but the hope of IPT-G is that by talking about our relationships with a group of peers, each person can contribute their own wisdom as well as learn from the wisdom of their fellows.”
In other words, HUGPT somewhat resembles the group Johns joined in that it is centered around interpersonal relationships, though with a secular communal dimension, rather than a religious one.
I did not attend the group out of respect for the privacy of its members. But I spoke with one of its founders, Suhaas M. Bhat ’23-’24, who has long dreamt of what he terms a peer group “therapeutic church” — something that would reside at the intersection of peer therapy, community support, and spirituality.
“In high school, I was a sad boy,” he says, laughing, before delving into his early struggles with depression and anxiety and his experiences with CBT. This oscillation between humor and gravitas characterizes the rest of the conversation.

During his first semester of college, Bhat had recently gotten out of his first relationship, and was tasked with making new friends and figuring out what he wanted his college experience to look like. “Saying goodbye to a version of myself took place over that semester,” he says. “I drowned myself in work.”
As a member of Harvard’s chapter of Effective Altruism, a movement and philosophy aimed at improving the world, Bhat learned about StrongMinds, an organization in Uganda that provides peer-facilitated psychotherapy to women. StrongMinds has treated 140,000 women for depression, with low relapse rates and a cost of only about $50 per woman for the entire course of treatment.
Inspired by this model, Bhat and his fellow EA member Eric H. Li ’23-24 envisioned a scalable, accessible peer group therapy program for Harvard students.
After meeting with CAMHS and receiving six months of training from the Interpersonal Psychotherapy Institute, Bhat and Li launched HUGPT in the fall of 2021.
Bhat and Li see their group as a less intimidating alternative to professional therapy. As their pubbing email reads: “Formal therapy can feel daunting but imagine a clinically-validated therapy (no cost or insurance required) where you talk through what's on your mind with people who understand. HUGPT is a safe space where students support each other in building healthy and fulfilling relationships that can meaningfully reduce depression and anxiety.”
Peer group therapy has the potential to address the supply-side issues Hyman raised, by broadening the care suppliers beyond licensed therapists and enabling the proliferation of training. “There are a lot of people who want to provide care for each other. You don’t have to be a special person to do that,” Bhat says. “Few people don’t want to take care of each other.” Rather than position some peers as counselors and some as patients, everyone in the group cares for and is cared for by one another.
Bhat synthesizes the more spiritual aspects of care Johns discussed with a secular idea of community. Early in our conversation, I confide in him my growing skepticism towards therapy. “Therapy is not the end-all, be-all. Therapy is our cultural substitute for religion,” he argues. “Group therapy is useful because it facilitates a sense of community and support.”
Ultimately, Bhat envisions peer therapy as part of a broader move toward “proactive therapeutic care instead of reactive care,” he says. “Currently the way we do care is that we wait for something really bad, then we get you a therapist … Check-ups instead of surgeries makes things easier.”
His ideal: Upon admission to Harvard, every student would receive an intake, an initial assessment to determine if they need care. If they need more intensive treatment, they can get it. If they want to join a peer group, there’s a pipeline for that, too. But in general, proactivity is institutionalized, so students no longer feel that the onus is on them to secure care.
Bhat hopes to expand HUGPT on campus and spark similar movements at peer institutions. But it’s worth noting that his group, like the other peer therapy organizations, has struggled to recruit and retain students. “The hardest thing was and continues to be getting high volumes,” he says. “Because there’s something scary about going to a group of people and baring your soul.”
Bhat’s expansive communal model of mental healthcare, one based in endogenous rather than exogenous care, resonates with me. Beyond peer therapy, I wonder what other forms of community support exist on campus, and how they could be expanded.
***
Ninety-eight percent of undergraduates live in the upperclassmen houses. Bhat callsed the house system “the true social organizer of Harvard.” And when I applied to Harvard, the houses were a big draw.
I’ll be honest, though: In my time here, I’ve never seen the houses as a center of my social or emotional life. Aside from eating, sleeping, and working, I’ve spent very little time in my house; I've barely interacted with my tutors or house committee.
But much of the scaffolding for communal care already exists in the upperclassmen house system: Resident tutors and house deans are on call to help students, and the wellness tutors program, which began in 2004, has since expanded to offer care for mental health issues and more. The Cabot House website’s Wellness page lists components of wellness, such as managing stress, anxiety, depression, sleep deprivation, and questions of religion and faith; the wellness tutors serve as “point people for any concerns, questions or requests you might have to help you live a better, fuller, and more balanced life.”
In mid April, after struggling through nights of insomnia, my roommate Vicki Xu ’23-'24, a Crimson Magazine writer, called the HUHS hotline and was eventually connected to a resident tutor in Currier House. He talked to her for about half an hour. An hour later, she was able to go to sleep.
After a few days, the resident tutor followed up over email, offering to talk about sleeping and rest tips. Xu’s house dean also reached out.
Xu was surprised that her house had become the nexus of mental health care she received. “I honestly didn’t think of it as a possibility,” she says. “It just didn’t cross my mind.” But as a Peer Advising Fellow for freshmen herself, she’s familiar with some of the protocol for this in freshman dorms and entryways, she says.

This gap in support between freshman year and upperclassmen housing extends beyond her experience. According to the 2020 Mental Health Task Force report, students saw the freshman year system of advisors, proctors, and PAFs as a “major strength” but felt that “this system of support largely disappears once they move into the Houses.” The report also notes that houses differed in the range and quality of support offered, and that tutors and proctors are “unclear or facing changing expectations about their role in recognizing and responding to serious mental health issues among their students.”
A stronger, clearer role for the houses in mental health care could be part of a proactive effort to take some of the burden off of professional therapy. “CAMHS used to say there’s no problem too small. But with overwhelming need, there has to be more support prior to seeking professional help,” Lewis says.
In the meantime, Xu has been attending the Currier House wellness study breaks, which involve making tea and doing guided meditations. “I do think it is important that when something like this happens, the tutors and deans check in on you,” she says.
***
In taking my inventory of available mental healthcare for students, I tried to evaluate each component’s strengths and limitations, in an effort to imagine how, together, they might form an effective mosaic of care. Still, I found the overall network insufficient — for people with severe mental health issues, there’s a shortage of therapists, and for people with less pressing concerns, there were still too many ways to fall through the cracks. Even I had trouble as I poured more time into these efforts than most students have to spare.
Taboo around discussing mental health persists, as illustrated by my conversation with my friend, as well as my difficulty finding people to speak about their mental health on the record. But in the interviews I did get to conduct, mental health care was spoken about candidly as a responsible and reasonable treatment to seek, something that could be discussed with friends.
To me this suggests that we’ve progressed through some de-stigmatization, such that we feel more comfortable encouraging people to get therapy. The tricky part is balancing that de-stigmatization with the understanding that therapy is not a panacea, and it’s far from an unlimited resource. Calls for CAMHS to simply bulk up are misguided: Even with added funding, CAMHS can never expand to the extent that every student could have immediate access to a licensed clinician — and along the way, such an expansion would take therapists from the surrounding community, away from people who are no less deserving of therapy than Harvard students.
And while students demand more CAMHS therapists, the peer groups remain underused, which I see as evidence that valorizing therapy has cost us our faith in our peers’ ability to care for us. I count myself guilty in this; although I found my time at peer therapy cathartic, at no point did I completely overcome my skepticism about its efficacy.
To be clear: Some people need and benefit from therapy done by a professionally trained, licensed clinician. I do not mean to diminish the value of therapy, especially for people with severe mental illness for whom it can be life-saving. And I want to reiterate the limitations of my own experience, as someone who stands to benefit less from care.
But there seems to be a belief that no matter what your problem is, some form of professional therapy will work for you. And that is not the case: Many of the people I spoke with found that therapy wasn’t compatible with their needs. So “you should try CAMHS” simply does not cut it.
In sum: While therapy can be crucial for some, increased, professional one-on-one therapy is not — and cannot be — the answer to all of our mental health woes. Instead, there needs to be a more radical reimagining of mental health care that includes therapy but extends beyond it, one that centers community and relationships and builds on existing campus infrastructure — a more tightly woven safety net that catches people before they need professional help. Maybe that looks like an expanded version of Bhat’s peer group, or a bolstered house-life-centered system. But it could also be something unexpected and different.
***
As for me, I’ve been taking an ornithology class this semester, which has required me to go birdwatching many weekend mornings with classmates. I also spent spring break with these classmates on a class trip to a few wildlife refuges on the gulf coast of Texas. We’ve seen a lot of birds. Mostly we’ve seen one another: We’ve slept inches apart, eaten meals together, huddled in early morning when it was cool and shared water when it was hot. We’ve talked about friendships, relationships, anxiety, and God. They, more than anyone, have helped me come to terms with the end of a friendship. In many ways, it’s been a lot like Bhat’s peer group: a set of relative strangers recurrently convening in an insulated space, supporting each other mentally and emotionally.
My birds class has offered the aspects of care I’ve come to see as crucial: It’s built into life in an integrated academic-social way; it’s mutually supportive, sustained, and permeated by a greater, even ineffable, sense of belonging.
I don’t give this as an example of a replacement for professional therapy, or something that would work for everyone. But for me, it’s consoling to feel that beyond the bounds of close friendships, and outside of the therapist’s office, there exists the possibility of a more universal care.
— Magazine writer Talia M. Blatt can be reached at talia.blatt@thecrimson.com. Follow her on Twitter @talia_m_blatt.